
As we know all too well, as many as one in four pregnancies will end in miscarriage, the majority of these within the first 12 weeks. In this interview, Genea fertility specialist Dr Anthony Marren shares his insights and experience of how GPs can best support patients through miscarriage, pregnancy loss and beyond.
Pink Elephants and Genea have formed a partnership. Why is it so important?
Pregnancy loss is quite a distressing time for couples and Genea, along with Pink Elephants, is passionate about opening up the conversation around it and trying to support women and couples through what is a very difficult time.
As GPs on the front line, we are often having the hard discussions about miscarriage. One of the hardest things to talk about is the ‘why’. What are some of the reasons that people might be experiencing these early pregnancy losses?
Firstly, I think it’s important to say that the rate of pregnancy loss increases with a woman’s age. So when the woman is in her 20s and early 30s, it’s around 15% per pregnancy and then it starts to climb after 35, and certainly once you hit about 45, around 90% of pregnancies are unfortunately lost.
Secondly, what we tend to see is something called a clinical pregnancy loss where a woman has missed a period and has gotten to the stage of a scan and the pregnancy is lost on scan. There’s a whole lot of pregnancy loss that occurs much earlier on in the piece. These are early implantations that fail, and we often talk about an iceberg effect where we only see the tip of all the pregnancy losses that actually occur.
So the pregnancy is lost before they even knew they were pregnant?
Yes, that’s correct. I think most pregnancy losses when they’re just a once off, we’ll never truly know the reason why, but most likely it’s due to a chromosomal error in the pregnancy itself and essentially the pregnancy fails at a certain stage and then the pregnancy is passed. So for one-off or sporadic losses it’s most likely to be an embryo issue, again chromosomal, whereas when it becomes recurrent, other factors tend to be at play.
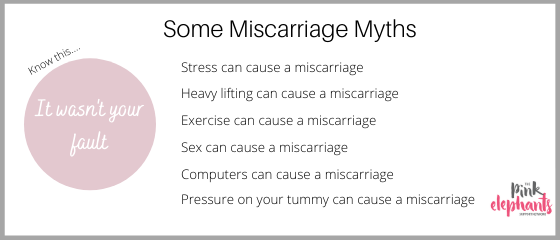
When I’m talking to patients I tend to say that it’s almost impossible to bring on a miscarriage? Is that correct?
Yes, I would tend to agree. I think a lot of women will look at what they’ve done and try to blame themselves, and it is near impossible to cause a miscarriage. There are studies that have looked at stress and pregnancy loss and the data we have would suggest that stress doesn’t lead to an increased miscarriage rate. The only thing that may have an impact is say if someone was really unwell with a flu like illness and had a really high temperature, then it may lead to a miscarriage but that’s not saying that the patient themselves is causing it.
So as GPs, when should we consider the necessity to refer a couple on to a specialist such as yourself?
The definition of recurrent pregnancy loss has changed over the years. It was traditionally defined as three pregnancy losses and if you use that definition, you end up investigating about 1% of the population and can generally uncover a cause in about half to two-thirds of cases.
Due to the stress that pregnancy loss causes, nearly all of the international guidelines have shifted and they’re now suggesting that we offer investigation after two miscarriages. This means investigating about 5% of the population and uncovering a cause in just under half. However after two losses, many people are quite concerned about what’s going to happen with the next pregnancy and they’ll often be more than happy to have those investigations. If they’re all normal then you can reassure them that it’s safe to continue trying to conceive.
Does age come into that? Should it be after three when a woman is younger and after two when they’re older?
Probably not to be honest because if someone is quite young, the risk of chromosomal error is less. Therefore if they’ve had two losses, they might be at a higher risk of something else going on in the background. The other thing I’d say is that if someone has a late loss and by that I mean, a loss that is beyond 10 weeks of proven ultrasound viability, they should really even be tested after one, because it’s quite unusual to miscarry a pregnancy after 10 weeks.
And are there things we can do or investigations we can request that will assist you, before we refer a couple on to you?
Yes definitely. In terms of causes of recurrent pregnancy loss, one of the things we want to do is to get a karyotype of both people in the couple. It’s also not a bad idea if possible, that when a woman is having a miscarriage, she could collect some of the tissue. Obviously this will be difficult for some people, but a lot are happy to do it because it has the potential to give them answers. The retrieved tissue just needs to be stored in a clean jar and put in the fridge until it’s taken to a pathology centre. This way a karyotype of the products of conception can also be done. The karyotype results are really quite important, but they also take around 6 – 8 weeks to come back, so it’s helpful to get that investigation done relatively early.

As GPs that would be a difficult conversation to be having with our patients…
Yes, it may feel insensitive to suggest, but if the woman has already had a couple of pregnancy losses, and they are able to collect some tissue, then it really does help as it give us a reason as to why the pregnancy loss has occurred.
For instance, if it comes back as a Trisomy 16, then it’s clearly a chromosomal issue and it gives them answer. Whereas if they have miscarried a chromosomally normal pregnancy, it’s a bit unusual and it means you’re more like to find something else in another investigation.
The other investigations that can be really helpful are a good quality ultrasound where they have a thorough look at the uterine anatomy. I would suggest a 3-dimensional reconstruction of the uterine cavity plus also a test called a sonohysterogram where the ultrasound technician injects a little bit of fluid into the uterus. That would probably be the standard of investigation now to look for uterine abnormalities that are either congenital such as a uterine septum or acquired such as a polyp or a fibroid.
So there’s a lot that we could potentially do to help you at the end of the day.
Yes, and some of these investigations can take a little bit of time, so if the couple arrive at their first appointment and the routine tests that we would normally do have been done, then we can have a far more meaningful conversation straight up and also they’re not then waiting another 6-8 weeks for a karyotype result to come back and delaying any potential treatment further.
When it comes to the imaging, is it worthwhile referring our patients to a specialist women’s health and obstetrics imaging practice?
Without a doubt. The specialist centres are usually obstetricians and gynaecologists who have done additional training in obstetric and gynae ultrasound and that’s all they do. They also have a clinical background so will know what’s relevant and what’s not and the report that you get from them is far more informative than a lot of the reports that you’d get from a general ultrasound or radiology practice.

So as GPs there’s a lot we can do to prepare the patient to get to you, but then what happens? What sort of treatments are available?
I think if someone’s had three losses, we would expect to find an underlying cause in about half to two-thirds of cases. If someone’s had two losses, we’d find a cause in just under half.
In the group where it’s unexplained, what’s really important there is that all of the investigations are normal. Data would tell us if these women go on to achieve another pregnancy, the most likely outcome will be a positive one. Often those couples will need a bit more support and reassurance with the next pregnancy. Some additional pregnancy hormone and progesterone levels, an early ultrasound and that TLC care, which in itself has been shown to be advantageous.
In terms of if something is found, for example if there’s a uterine septum on an ultrasound, then obviously we’re going to be directing our treatment specifically to that. We’d be talking about a hysteroscopic procedure and division of septum. Or if one of the thrombophilias is positive, then we’ll discuss some kind of anticoagulation in the pregnancy, whether or not that’s low molecular weight heparin plus or minus some aspirin and so forth.
In each of the tests we do, we’re basically looking for a specific cause and by and large there’s a treatment for it.

Another term that I’m seeing used a lot more now is this pre-implantation screening. How does that fit in and how does it help reduce miscarriage rates?
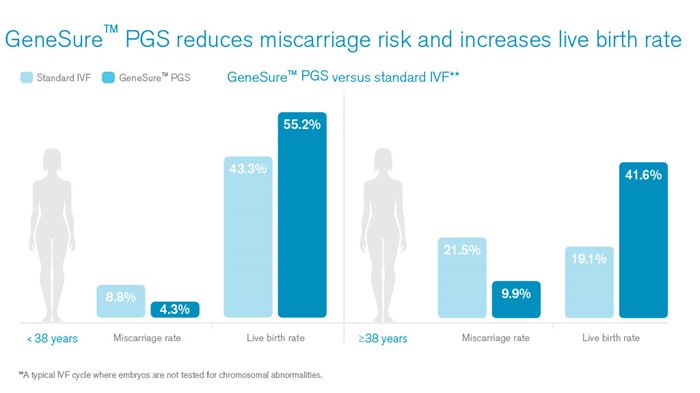
As a woman gets older, the rate of chromosomal errors in the egg increases and it’s this that leads to a reduction in fertility and an increase in miscarriage. For instance, if couples do a cycle of IVF and they get embryos tested, the rate of chromosomal error is related directly to the age of the woman, and in our young population, less than 35, about 30% of those embryos are going to be abnormal. However, once you come up to about 43 or 44, then about 80 or 90% of those embryos will be abnormal, which is significant.
If you’ve got someone whose had a few pregnancy losses and all of the screening that’s been done is normal, the uterus is normal, there’s no thrombophilia and particularly if you’ve tested one of the pregnancies and there was a chromosomal error, then it’s likely that those women are having recurrent pregnancy loss due to recurrent chromosomal error.
If you can take those women through an IVF cycle and get embryos tested, and you manage to get a normal embryo to transfer, then it should implant somewhere between 50-60% of cases. The miscarriage rate also becomes very low, less than 5%. So the advantage of that is you can reduce the psychological burden of recurrent miscarriage.
The other factor is that if a woman falls pregnant, gets to say 8 weeks and then finds out it’s a miscarriage, have a procedure and then wait 4-6 weeks for their period to come back, ultimately it ends up being a few months before that woman or couple is able to try again. And if the woman is 41 or 42 and she loses 4-6 months each time there’s a miscarriage, that will really disadvantage her in her ability to achieve a successful outcome. So embryo testing is really about finding that embryo that is going to give the greatest chance of implantation and the lowest risk of miscarriage.
And is that what GeneSure is about?
Correct. It’s basically at the day 5 or 6 stage where the embryo is over 100 cells and we take about 5 cells that go on to form the future placenta. We biopsy those and we amplify up the genetic material and we screen it and look at all of the chromosomes. We’re not just looking at say chromosome 13, 18, 21, we’re looking at all of the chromosomes and we sort the embryos out into those that are chromosomally normal and those that are not.
What sets that process apart at Genea?
Certainly in Australia we were one of the first if not the first company to grow embryos through to day 5 which is now the world standard. In our lab, our day surgery and lab is open 7 days a week, so we can perform our egg collection when we think those woman’s ovaries are ready to actually have the egg collection process, so we’re not restricted to certain days of the week like other clinics.
The other important thing is that our genetics lab is within our actual centre, so we’re not sending cells interstate or overseas. The woman will have her egg collection at the right time, the embryos are biopsied at the right time, all of the genetic material is tested on site and we are comfortable that we’re giving our patients the best chance of having a successful outcome.
I’m just wondering about blokes. Where do they fit into the miscarriage issue?
Obviously we want a chromosome blood test on them as well. The other thing is from a semen analysis perspective, the basic semen analysis looks at the number of sperm, how they move and their shape. The other thing that’s important in terms of miscarriage is DNA Fragmentation. Essentially the genetic material is packaged inside the head of the sperm and from the time that sperm start to be produced to the time that it’s released is roughly 70 days. And during that time it gets exposed to heat and toxins, for instance if the guy smokes, and so that genetic material can be damaged. And if that DNA Fragmentation is high, then it is associated with an increase in pregnancy loss.
So firstly we look at lifestyle things. If they are smoking we’d get them to stop, if they do lots of running or cycling then the temperature is probably not great for the testes so we ask them to modify that. We introduce things like antioxidants, like vitamin C and zinc, we get more regular ejaculation so that the sperm that’s used around the time of fertilisation is as fresh as it can be. And certainly if the couple are doing IVF we actually have some advanced sperm selection techniques to choose the better sperm to bring with the egg if DNA fragmentation is an issue.
It’s for this reason it’s really important to see the couple, not just the female. There’s no point in subjecting the female to all sorts of investigations, some of which are relatively invasive, but ignore half the equation.

What other strategies that you see that Genea has to support patients experiencing miscarriage?
Obviously there’s the support that happens at the specialist level, so the couple should be appropriately worked up, the underlying problem should be discussed and also a range of treatment options should be presented. For those that are then going to undergo fertility treatment, we have teams of doctors with nurses, so I have a couple of nurses that just work with me and they know my patients just as well as I do really, and those nurses are incredibly supportive. They do a lot of the communication with the patients, they are the ones who are often talking to the patients every couple of days and relaying results etc.
The other thing is that we have three counsellors that work with us in Sydney and those counsellors have a wealth of knowledge and experience in couples with underlying fertility problems and also pregnancy loss. So we always make sure that the patients are aware that the counsellors exist. If we can see that the patients are struggling, we’ll get the counsellors to contact them straight up. Otherwise we’ll just give the counsellors number to the patients and they can choose to make contact with them if they want.
The main thing at Genea is that it’s not just one person doing everything, it’s a team based approach from the specialists, the nurses and the counsellors.
When is it safe for patients to try to conceive again after they’ve had a miscarriage?
After a miscarriage they should have one completely normal period and then they can start to try. For instance if someone spontaneously miscarries or has a curette, then after their next normal period they can try. There was some old data about waiting for 3 months but there’s no evidence for that. However if a couple do achieve a pregnancy before the next normal period, that pregnancy is at a slightly increased risk of miscarriage.
To finish up I’m going to put you on the spot. I’m wondering if you’ve got one key message that GPs can pass on to their patients who are worried about miscarriage.
This is really for the patients who are being investigated. If they’ve had a couple of losses and all of the investigations are normal, the key message is not to be fearful about having another pregnancy. If couples have had three pregnancy losses and everything is normal, 70-80% of their next pregnancies are going to be completely fine. So it’s really important that they’re not fearful. The GPs will support them. The specialists will support them, but they should go away and try and achieve another pregnancy.
Link to the original podcast:
https://www.genea.com.au/hcp/baby-steps-podcast
